A group of researchers from the Federal University of Paraná (UFPR) examined the presence of the genetic material for the Coronavirus in Curitiba’s public health settings. The results are published in the International Journal of Environmental Research and Public Health. The work was supported by the Higher Education Personnel Improvement Coordination (Capes), the National Council for Scientific and Technological Development (CNPq) and the Municipal Health Secretariat of Curitiba (SMS). 711 samples were collected in four basic health units (in the Boa Vista, Bairro Alto, Kajuro and Cabau da Empoya neighborhoods); In the Boa Vista Emergency Care Unit (UPA) and at the Hospitals de Clinicas and Piceno Principe.
In base units and at UPA, there have been clusters in dental units, physician offices, and evaluation units for Covid-19. In hospitals, the analysis was performed in intensive care units (ICUs) and wards to care for patients with the disease. This is the first public health environmental analysis study to include dental services. “We wanted to understand how the virus could spread in hospital settings, compared to basic health units and dental places,” explains Professor Vânia Vicente, from the Department of Basic Pathology. The research was prompted by a request from the agencies in charge of the devices, says Vivienne de Souza Joubert, from Coordinating Oral Health in SMS. “We were very interested in how SARS-CoV-2 performed in the dental environment. Everything was very new and we had doubts about the routine procedures in the clinic.”
The viral RNA collections, which were performed during the second half of 2020, were performed by swabs, in a similar manner to the tests for detection of the Coronavirus. “We chose a chemical inactivation with an enzymatic detergent, and in the laboratory, the genetic material was extracted from the entire environmental sample,” says UFPR University’s bioprocess and biotechnology student Maria Eduarda Grisolia.
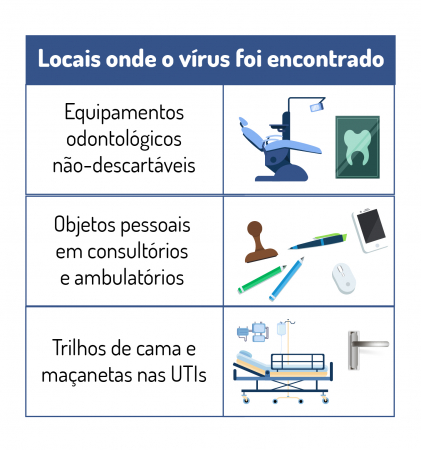
In 234 samples in dental settings, there was a positive rate of 3%. Although the results are consistent with the rates presented in other studies already conducted, the team highlights the stability of RNA in dental materials that cannot be disposed of, such as reflectors and saliva repellents. In some cases, samples that are positive for SARS-CoV-2 RNA have been found in the dental chair, even after the device has been cleaned, enhancing the rigor to be followed during the disinfection process.
RT-PCR positivity in samples collected in the outpatient setting was greater than in some hospital settings. Example: Of the 85 dispensary samples, viral RNA was detected in 9% of the sites. In medical offices, viral RNA has been detected in personal items, such as pens, stamps, and notebooks. Additionally, doorknobs, computer keyboards, mice, armchairs, and oximeters were positive for SARS-CoV-2.
The study also showed that door handles and bed rails were the most contaminated surfaces in ICUs, with a rate of 14% and 22% of positive samples respectively.
In the Covid-19 evaluation unit, viral RNA has been detected in keyboards, mice, oximeter, thermometer, patient chair, door handle, and in X-ray equipment where a patient immobilizes their chin for testing. Of the 711 samples analyzed, 35 were RT-PCR positive for SARS-CoV-2.
Disinfection and prevention
The team explains that this work does not determine the viability of the virus, meaning that the presence of the virus’s genetic material in the environment does not necessarily mean that people can be contaminated. This depends on a number of factors, ranging from cleaning the environment to how long the virus has stayed in that location.
However, the data indicate that these are critical points and that at some point, the virus may be viable in those locations. Hence, it is an important indicator that reveals the need for more stringent disinfection measures in these areas.
In addition, the numbers indicate that the virus is spreading in health units not designated for treating Covid-19. “Despite being in control, wearing masks and disinfected environments, there are people with Covid who transmit the virus,” says Bruno Paulo Rodrigues Lustosa, a student in bioprocess engineering and biotechnology at UFPR who participated in the groups.
In this context, Professor Sonia Raponi, Senior Infection Specialist at Hospital de Clinicas, points out that we are in a period of pandemic, with a high rate of transmission of this new pathogen in the community. “A large proportion of the infected have no symptoms or have mild, nonspecific symptoms. In this way, these individuals continue to have their usual clinical and dental consultations and can be sources of contamination of the equipment, professionals or patients who will be treated in these settings.”
The infection specialist also notes the need for teams to work with these patients, regardless of the presence of symptoms, to step up preventive measures. In addition to environmental pollution, other factors are necessary for disease transmission, such as proximity and contact between infected and uninfected people. It is clear in screening studies that there is a need for the presence of an infected person and that contact occurs without the recommended preventive measures, ie: without moving away, wearing a mask and proper hand hygiene.
According to Professor Vania, the results reinforce the idea that virus control is multifactorial. “We have to surround ourselves on all fronts. In addition to immunization and wearing a mask, we also have to take care of our relationship with the environment. He concludes that during a pandemic, despite our isolation, we can get sick and therefore need health services.”
Also participating in the article were researchers Caroline Pavini Pitto, Eduardo Balsanelli, Miri Bordinion Nogueira, Catherine Athide Teixeira Carvallo, Isadora Servilien Fleur, Morgana Ferreira Vojaleschi, Ramiro Gonsalves Echbari, Jacques F. Mays, Vanity Tomas Sokol and Emanuel.
Other indications
The team is continuing its environmental investigation to determine, through genotyping, which strains circulate in different environments. For now, researchers are also focusing on another indicator: SARS-CoV-2 monitoring in wastewater by RT – PCR. The research is taking place on a national network, through a joint initiative between the National Water Agency and the National Institute of Science and Technology of Sustainable Wastewater Treatment Plants, at the Federal University of Minas Gerais.
The project is coordinated by Professor Carlos Augusto de Lemos Cirmicharo, of the UFMG, and includes several educational and research institutions, including UFPR. The local coordinator in the Parana nucleus is Professor Ramiro Gonçalves Ichibar, from the Hydraulics and Sanitation Department.
Research is ongoing and results will be released soon. Professor Emmanuel says: “This indicator represents a picture of the societal turnover of the virus, and thus, can provide warning signals for decision-making on restrictive measures.”

“Wannabe internet buff. Future teen idol. Hardcore zombie guru. Gamer. Avid creator. Entrepreneur. Bacon ninja.”